Despite recent investment, waiting lists are at an all-time high. Consultant-led outpatient appointments provide an opportunity for patients to receive consultation, investigation and minor treatment. Current demand is high, with over 1.5 million outpatient appointments occurring each year. Some clinical specialities have long waiting lists, resulting in patients experiencing significant delays to get treatment. This in turn can have a detrimental impact on their health and well-being.
Incomplete waiting time data
Outpatient waiting times are measured from the date a Health and Social Care Trust receives a referral for a patient, usually from a G.P., and ends when the patient attends their first appointment. Review appointment waiting times are not measured. Instead, a separate waiting time ‘clock’ begins if the patient requires treatment as an inpatient, for a diagnostic test, or a day case admission. However, this data is not linked. Therefore it is impossible to know if patients are being seen and treated in a timely manner. Likewise, it is not possible to make meaningful comparisons against performance across the UK – where more complete outpatient journey times from referral to treatment are collected.
Numbers waiting
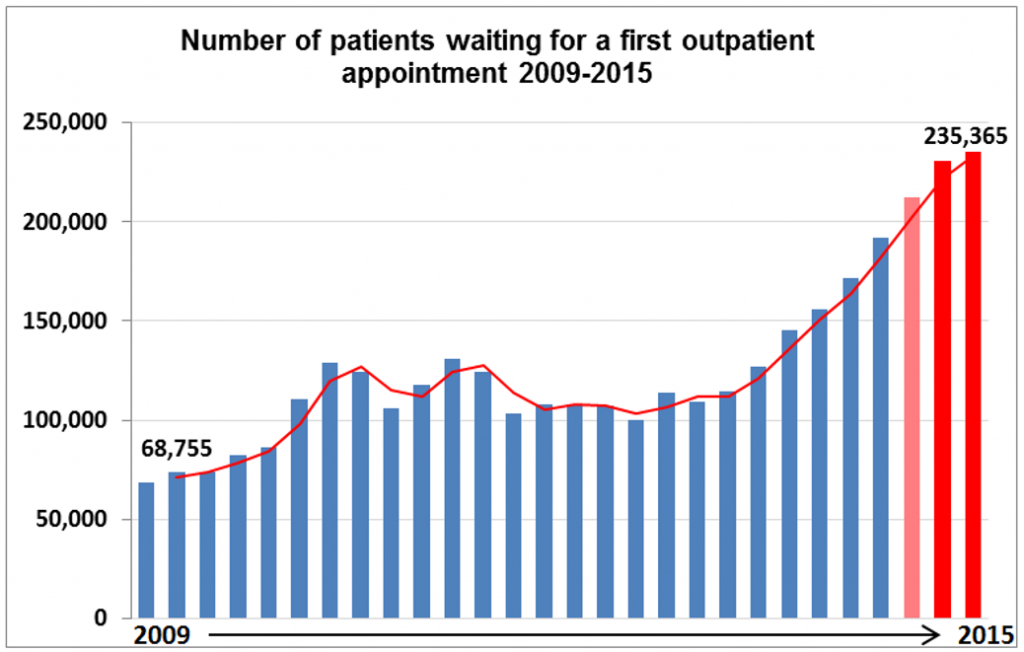
The Department of Health, Social Services and Public Safety (DHSSPS) reports on the number of people waiting for their first outpatient appointment on a quarterly basis. As can be seen in Table 1, the number of people waiting for a first outpatient appointment has been increasing in Northern Ireland over the last six years. These reached unprecedented levels in December 2015 when around 235,000 patients were waiting. This is more than treble the number of outpatients that were waiting for a first appointment in 2009 (see Figure 1).
Ministerial targets
In order to monitor the performance and efficiency of outpatient services, outpatient waiting times in Northern Ireland have targets attached to them, as shown in Table 1. Targets are determined annually by the Minister for Health within the Health and Social Care Commissioning Plan Direction for Northern Ireland. These specify the maximum amount of time that patients should expect to wait for their first outpatient appointment. Yet no other jurisdiction in the UK has set targets in this way, nor changed them as frequently as here in Northern Ireland.
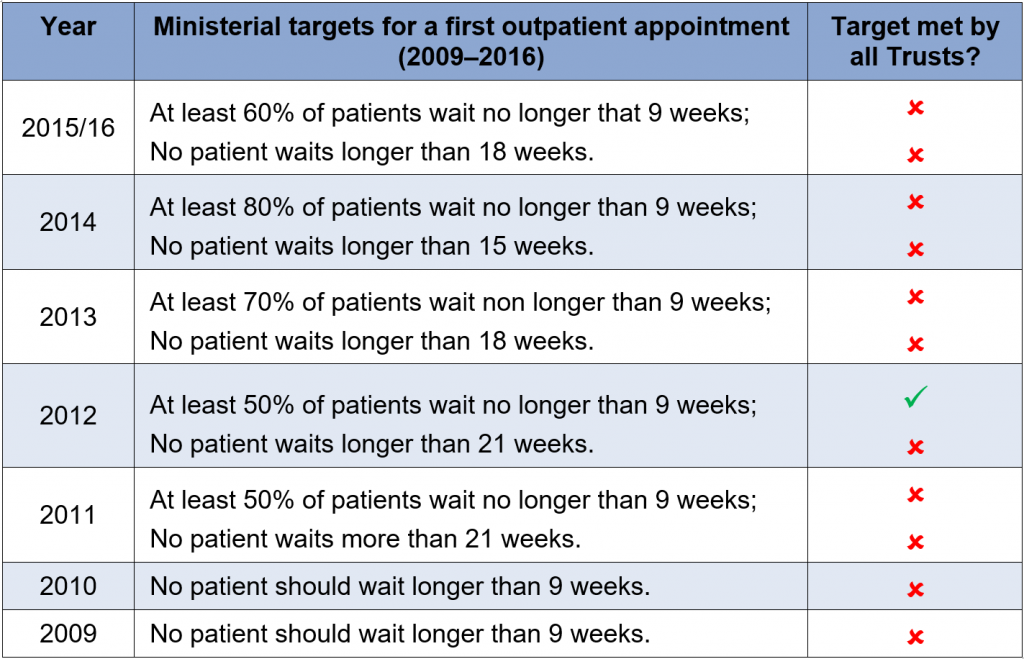
As can be seen from Table 1, performance against the targets has not been met. This raises a number of questions such as:
- What is the value of having targets that get missed repeatedly?
- Why are more meaningful targets or measures not being adopted?
Clinical specialties with the longest waiters
The current 2015/16 outpatient waiting time target states that ‘no patient should wait longer than 18 weeks for a first outpatient appointment’. Data from the Department indicates that in June 2015, 85,997 (40% of all patients waiting) had been waiting more than the maximum time of 18 weeks. Furthermore, nearly 900 of them had been waiting over 18 months (not weeks) to be seen.
By the end of December 2015, the number of patients waiting over 18 weeks had risen to 122,771. Over half of these patients were waiting for treatment in one of the following clinical specialities: trauma and orthopaedic surgery; ear, nose and throat; general surgery; ophthalmology; or neurology.
Factors impacting on waiting times
The waiting times issue is not new, nor is it unique to Northern Ireland. Several complex and inter-related factors have contributed to the high volume of outpatients waiting and the lengthy timeframe some of them are waiting. These include:
- Funding constraints – given the current fiscal climate and the restricted budget that the Department has to live within.
- Patient demand outstripping capacity – given factors such as the increasing ageing population, and the rise of more complex chronic conditions.
- Strain on other parts of the healthcare system.
- Reduction in use of the independent/private sector.
- Continued reliance on Monitoring Round monies.
- Staff recruitment and retention problems.
- Lost productivity – for example, in 2014/15 hospital providers cancelled 168,555 outpatient appointments and patients missed 147,536 outpatient appointments.
What action is being taken?
In 2014, the Northern Ireland Assembly’s Committee for Health, Social Services and Public Safety undertook a Review of Waiting Times. Its Review report made several recommendations including:
- Introducing a system to measure Referral to Treatment times and targets;
- New arrangements for managing Trust performance; and
- A clearly defined policy on how compliance against the targets will be enforced.
Despite these recommendations, current outpatient Ministerial targets remain in place and no new system to measure waiting times has been developed. Instead, the Department has recently invested over £70 million in order to increase activity to tackle growing waiting list pressures. The Department has also introduced a range of initiatives such as the prioritisation of patients by clinical urgency; chronological management of non-urgent patients; regularly informing GPs of waiting times; and seeking new alternatives to face-to-face consultant-led outpatient appointments.
The latest provisional waiting time figures for outpatient appointments and admission for treatment as at the end of February 2016 show reductions compared to the end of December 2015. Those waiting more than nine weeks for a first outpatient appointment have fallen by over 14,000 and those waiting over 18 weeks, by over 11,000, around 9%. The Department has acknowledged that further change will take time and significant non-recurrent and recurrent investment to bring waiting times back to an acceptable level.
Whilst a lack of funding is a large part of the waiting times problem, investment alone will not resolve this issue. It is clear that there are also questions about how the system is being managed. With the dawning of the new mandate, it will be interesting to see if the Committee for Health’s recommendations on waiting times are realised, and if, or when, there will be a significant reduction in the number and length of time that outpatients are waiting.

