
This blog article is based on the information and analysis in the recently published Northern Ireland Assembly Research and Information Service paper, ‘Waiting lists and waiting times for Elective Care in Northern Ireland: Taking stock’.
Introduction – What is Elective Care?
Elective Care is care planned in advance for those whose condition requires a procedure or treatment that can be managed by placement on a waiting list (WL). It also includes diagnostic services – medical tests to aid in the diagnosis of disease and assist in the management of patient care.
Elective surgeries aim to improve quality of life either physically (for example, cataract surgery or a hip replacement) and/or psychologically (for example, reconstructive surgery). Some elective surgeries may extend the life of the patient (for example, non-emergency cardiovascular surgery).
Key concerns
In Northern Ireland (NI), the numbers of patients on the Elective Care WLs and the waiting time (WT) to be assessed, diagnosed and treated is of mounting concern.
At the end of September 2019, there were just over 306,000 patients waiting for a first outpatient appointment and over 105,000 of these patients were waiting more than 52 weeks for that appointment.
For patients, the key concern is the time spent waiting. What is considered ‘too long’ a wait can be subjective to an individual patient depending on the impact their condition is having on quality of life, ability to work, care for family etc.
However, it is also a clinical matter and, for some services, there is evidence linking longer WTs with poorer clinical outcomes.
Elective Care: Statistics and targets
In NI, quarterly WT and WL statistics are reported/published by the Department of Health based around waiting time targets set by the Health Minister for separate stages of the Elective Care patient pathway (outpatient waiters, diagnostic waiters and inpatient waiters).
The number of people waiting for Elective Care has substantially increased in NI since the mid-1990s. Decreases in the numbers waiting were achieved in the mid-2000s but the majority of these gains were lost within a few years.
The most recent statistics for NI were published at the end of December 2019 and refer to the numbers for the end of September 2019. They show:
- 306,180 patients waiting for a first outpatient appointment with over two thirds of these waiting beyond the 9 week target and many well beyond it (105,450 of these patients were waiting more than 52 weeks for a first outpatient appointment);
- 87,353 patients waiting for inpatient admission, with 70% of these waiting over 13 weeks, compared to 36,808 waiting for admission in December 2009 when 16% were waiting over 13 weeks; and
- 140,237 waiting for a diagnostic service, with 57% of these waiting over 9 weeks.
For comparison, back in December 2009 there were only just over 80,000 patients waiting for a first outpatient appointment and around 37,000 waiting for admission.
For longer-term comparisons, the research paper uses December figures going back to 2008 and presents a series of graphs for outpatient, diagnostic and inpatient waits. For example, Figure 1 below shows the totals waiting for first outpatient appointment and waits over 9 weeks: December 2008 to 2018.
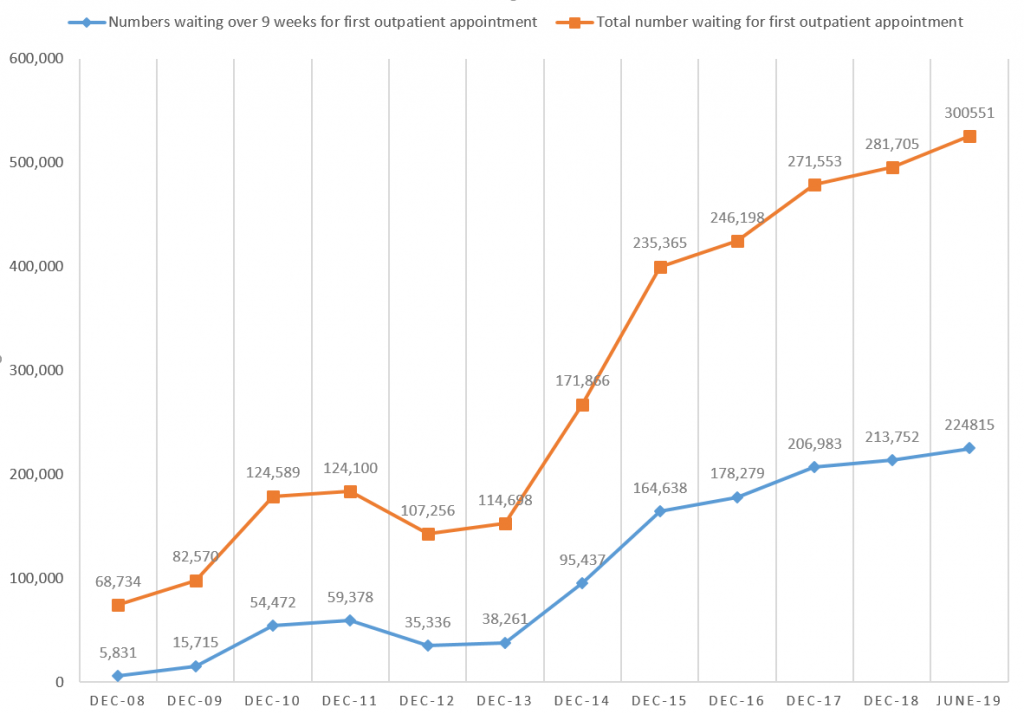
The outpatient and inpatient targets have not often been met since 2009. As waiting times and waiting lists have grown over the years, the targets have been changed to become less stringent. This raises the question of the purpose of the targets? For example, the current target for first outpatient appointment is ‘by March 2020, 50% of patients should wait no longer than 9 weeks with none waiting longer than 52 weeks’.
However, back in 2013 the target was that ‘from April 2013 at least 70% of patients should wait no longer than 9 weeks and no patient longer than 18 weeks’ and further back again in 2009 ‘from April 2009 no patient should wait longer than 9 weeks’ for a first outpatient appointment.
The entire patient journey time in the Elective Care system from referral to start of treatment (RTT), which is reported against related targets in England, Scotland and Wales, is not collated or reported in NI.
In NI, review appointments have no targets assigned to them and no waiting lists or times for these are published. This may be a significant gap as the Public Accounts Committee for the National Assembly for Wales has recently stated that ‘follow-up’ outpatient appointments are:
…the largest and most common form of contact between patients and healthcare services in an acute setting.
Reasons behind the increases
The main reasons behind the increases in waiting times in NI (over at least the past decade) in Elective Care are varied and include:
- Demand for Elective Care increasing with a year-on-year increase in referrals;
- Capacity to see and treat patients unable to keep pace with the demand due to limited resources available in-year to invest in additional in-house and independent sector waiting list activity;
- Agreed volumes of funded activity not being fully delivered by the HSC Trusts across a range of specialties;
- Postponement of Elective Care procedures due to increased unscheduled admissions to hospitals;
- A growing and ageing population; and
- Significant gaps across the HSC workforce.
Comparisons with England, Scotland and Wales
There is presently no way to directly compare NI’s Elective Care waiting time performance to anywhere else in the UK. The reason is that the current technology in the NI HSC system is unable to add together the separate stages of the patient Elective Care pathway to give the RTT time as used in the rest of the UK. Indeed, parts of the pathway in NI may not be recorded anywhere.
The new regional Encompass programme to introduce an integrated digital clinical record across the HSC should help in this regard going forward.
However, it is clear that NI is currently very slow at providing Elective Care compared to the rest of the UK. WTs and WLs have been rising in recent years across the UK. However, it is impossible to overstate the disparity between NI waiting times for Elective Care and the much shorter waits experienced by patients in England, Scotland and Wales.
For example, in England (total population around 55 million) at the end of November 2019 only 1,398 people were waiting more than 52 weeks on the Referral to Treatment (RTT) pathway to start treatment, whereas in NI (total population around 1.9 million), at the end of September 2019, 108,582 people were waiting more than 52 weeks for their first outpatient appointment.
Compared to NI, Wales is the next worse performer in the UK with regard to Elective Care waiting times. Even so, it has been commented that a person here is at least 48 times as likely to wait more than a year for Elective Care compared to a person in Wales.
England, Scotland and Wales are all currently taking actions around Elective Care. For example, the future of Elective Care in England is linked to the new ‘NHS Long Term Plan’ (2019) and in connection with this, the NHS National Medical Director is reviewing the core set of NHS access standards.
Patient journey times through Elective Care in NI
For NI, at present, based on the Department’s published figures, we can only ‘guesstimate’ possible maximum full patient journey times through the Elective Care system. Such estimates indicate possible times from referral to start of treatment of over four years in some cases. This correlates with figures released by HSC Trusts to the media showing that waits of up to four years for a first outpatient appointment are not uncommon.
To introduce the RTT measure and associated targets was a NI Assembly Health Committee review recommendation five years ago to the Department of Health. At last, it seems to be gaining traction as stated in the New Decade, New Approach document recently published jointly by the British and Irish Governments:
The Executive will consider the scope for changing how waiting times are measured, to reflect the entire patient journey, from referral to treatment, with appropriate targets.
The Chief Executive of NHS England recently noted that although the specific type of RTT targets used in England, Scotland and Wales all vary somewhat, he stated that:
Northern Ireland does not have a way at all.
Policies and actions in NI
In NI the history of policies and actions to address issues within Elective Care and its waiting times and waiting lists go back around 20 years.
The most recent Departmental plan to tackle the issues here is the 2017 Elective Care Plan – Transformation and Reform of Elective Care Services, which stemmed from the overarching healthcare reform strategy Health and Wellbeing 2026 – Delivering Together.
However, the New Decade, New Approach document states that the NI Executive will now introduce a new action plan on waiting times.
The 2017 Plan highlights that pressures on the HSC’s capacity to respond to increasing demand for Elective Care have been building for years and acknowledges that attempts to tackle this in the past have often had a short-term focus.
Progress has been made on its six commitments, with related actions, and makes it clear that sustainable improvement is dependent on progress in the wider health care transformation. There is substantial emphasis on two key areas – the transfer of a growing range of procedures to Regional Assessment and Surgical Centres and a larger role for primary care so there are fewer referrals to secondary care.
Conclusion
It appears that over the past two decades, the Department of Health in NI has not been able to make sustained improvements in Elective Care WLs and WTs in anywhere as near a determined or consistent a manner as neighbouring jurisdictions.
The technology, to capture and report full patient RTT pathways here, only now appears to be catching up, with the relatively imminent roll-out of the Encompass Programme.
The impact of the implementation of the transformation agenda, the 2017 Elective Care Plan and the forthcoming Executive action plan on WLs referred to in New Decade New Approach, remains to be seen.

